INTRODUCTION
The GHSG-HD21 trial for newly diagnosed adult patients with advanced-stage classical Hodgkin lymphoma (AS-cHL) compares the BrECADD regimen (Brentuximab vedotin, etoposide, cyclophosphamide, doxorubicin, dacarbazine, dexamethasone) to eBEACOPP (bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, prednisone) in a PET adapted approach. Separate analyses of the co-primary endpoints for tolerability and efficacy demonstrated a significant and relevant reduction in treatment-related morbidity (TRMB) and non-inferiority of PFS, respectively. Here, we report the first combined comprehensive analysis of the primary endpoints of the HD21 trial.
METHODS
This international open-label phase III trial included adult patients aged ≤ 60 yrs with AS-cHL. Patients were randomized in a 1:1 ratio to PET2-guided 4-6 21-day cycles of either eBEACOPP or BrECADD. PET2 and PFS events were assessed by blinded panel review. At a planned interim analysis at 36 months follow-up, the efficacy endpoint PFS was determined in the ITT cohort comprising 1,482 patients (eBEACOPP n=740, and BrECADD n=742) while the safety endpoint TRMB was determined in 1,470 patients (BEACOPP n=732, and BrECADD n=738). Subgroup analyses were calculated with 95% confidence intervals (Cis). The trial was registered at clinicaltrials.gov (NCT02661503) and conducted according to ICH-GCP guidelines.
RESULTS
Between July 2016 and August 2020, we enrolled 1,500 patients from 9 countries across 233 trial sites. Actual median follow-up for this analysis was 40 months. Baseline characteristics were well balanced between treatment arms, median age was 34 yrs (range 18-61), and 47% were high-risk (international prognostic index IPS ≥ 3).
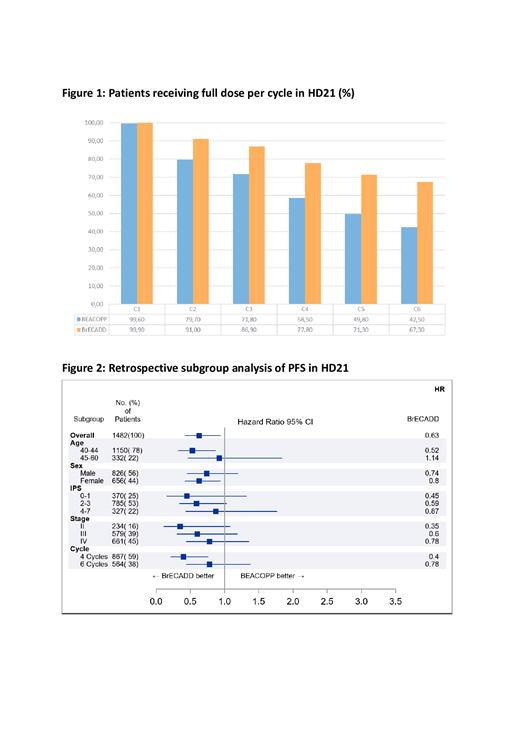
Overall, the relative risk for a TRMB event was 0.72 (95% CI, 0.65-0.79) in favor of BrECADD. Subgroup analyses confirmed a consistent, highly significant TRMB benefit in all relevant subgroups. Dose reductions were required less frequently with BrECADD than with eBEACOPP (figure 1); full dose treatment at cycle 4 was administered in 58.5% of patients in the eBEACOPP group compared to 77.8% in the BrECADD group. In PET2-positive patients at cycle 6, full dose treatment was received by 42.5% in the eBEACOPP group versus 67.3% in the BrECADD group. Most frequent reasons for dose reductions were leukopenia for eBEACOPP (in 33.7% of patients) and thrombocytopenia for BrECADD (in 23.1 % of patients).
59% of patients achieved a PET2-negative response and were treated with a total of 4 cycles in each group; conversely, 41% of patients were PET2-positive and received 6 cycles. At the end of treatment with either 4 or 6 cycles, a complete metabolic response was seen in 80% and 82% of patients in the eBEACOPP and BrECADD cohorts, respectively. The 3-yr PFS was 94.9% for BrECADD (95% CI 93.5% - 96.7%), and 92.3% for eBEACOPP (95% CI 90.3% - 94.3%), with a corresponding HR of 0.63 (95% CI 0.42-0.94). A HR favoring BrECADD was consistently observed across all relevant subgroups (figure 2). Notably, HRs favoring BrECADD were generally lower in lower-risk cohorts including IPS (0, 1; 2, 3; 4-7: HR 0.45, 0.59, 0.87, respectively), stage (Ann-Arbor stage II, III, IV: HR 0.35, 0.6, 0.78, respectively), or PET-2 response (negative versus positive, HR 0.4, 95% CI 0.21-0.76 vs 0.78, 95% CI 0.44-1.38). Corresponding 3-yr PFS rates for BrECADD versus eBEACOPP were 97.1% (95% CI 95.5% - 98.7%) versus 93.6% (95% CI 91.3% - 95.9%) for PET2-negative patients and 93.5% (95% CI 90.6% - 96.5%) versus 90.6% (95% CI 87.1% - 94.1%) for PET2-positive patients, respectively.
CONCLUSION
With the novel BrECADD regimen, we observed the highest 3-yr PFS rates reported to date in a randomized clinical trial in advanced-stage cHL. Our analyses suggest that the unexpectedly high and improved efficacy of the new BrECADD regimen compared to eBEACOPP is a direct consequence of its improved tolerability and deliverability. Importantly, while the larger patient cohort of PET2-negative patients achieves a very high 3-yr PFS of 97% with a very short and safe 12-week treatment, this benefit was also observed for PET2-positive patients. In conclusion, the optimized risk-benefit ratio of the BrECADD regimen combined with the individualized PET2-guided treatment duration sets a new benchmark for the treatment of adult patients with newly diagnosed advanced stage cHL
OffLabel Disclosure:
Borchmann:Bristol-Myers Squibb: Consultancy; Merck Sharp & Dohme: Consultancy, Research Funding; Roche: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Amgen: Consultancy, Research Funding; Takeda Oncology: Consultancy, Research Funding; MPI: Research Funding. Greil:Roche: Honoraria, Research Funding. Hänel:Novartis, SOBI, Gilead, Falk Foundation: Honoraria; Novartis, BMS/Celgene, Gilead, Pfizer, Incyte, Sanofi/Aventis, Roche, Amgen, SOBI, Janssen: Consultancy. Novak:Novartis: Other: Advisory Boards; Gilead: Other: Advisory Boards; BMS: Other: Advisory Board. Viardot:F. Hoffmann-La Roche Ltd, Abbvie, Kite/Gilead, BMS: Honoraria; BMS: Research Funding; F. Hoffmann-La Roche Ltd, Abbvie, Kite/Gilead, BMS: Consultancy. Giri:Royal Adelaide Hospital: Current Employment. Molin:MSD: Honoraria; Roche: Honoraria; BMS: Honoraria; Takeda: Honoraria. Ferdinandus:Roche: Honoraria. Hallek:Abbvie: Consultancy, Honoraria, Research Funding; Roche: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; AstraZeneca: Consultancy, Honoraria, Research Funding; BeiGene: Consultancy, Honoraria, Research Funding; Gilead: Consultancy, Honoraria, Research Funding.
USe of Brentuximab vedotin in combination with etoposide, cyclophosphamide, doxorubicin, dacarbazine, dexamethasone for advacned stage classical HL

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal